

Affiliations
ABSTRACT
Silicosis, one of the uncommon occupation-related lung diseases in Pakistan, is caused by long-term inhalation of crystalline silica particles. Progressive massive fibrosis (PMF) is a severe, not routinely encountered adverse outcome of silicosis, characterised by mass-like fibrotic opacities in the lungs. We report a case of a 38-year male, a stonecutter by profession, with a two-year history of exposure to silica, who developed silicosis, which in a couple of years led to PMF. The patient presented with low-grade fever, exacerbation of dyspnoea on exertion, chronic dry cough, and significant changes in radiology, evident on chest x-ray and high-resolution computed tomography. Conventional, supportive medical management was timely initiated; however, the patient's respiratory function deteriorated, emphasising the progressive nature and limited treatment options for advanced silicosis with PMF. This case report pinpoints the importance of early detection, prevention, and follow-up of individuals at risk for silicosis to reduce the probability of unwanted events.
Key Words: Silicosis, Progressive massive fibrosis, Occupational lung disease.
INTRODUCTION
Silicosis, a form of pneumoconiosis caused by inhaled particles of silica, is marked by the cascade of events resulting in inflammation and scarring, leading to the progressive accumulation of fibrotic nodules mostly in the upper lobes of the lungs.1 Recent evolution in the field of industrialisation has proven fruitful in the control and declining incidence of occupation-related health outcomes in the developed countries. In developing countries like Pakistan, due to lack of funding, resources, and public awareness, occupational health morbidities pose a major risk to health outcomes. The severity of the disease is directly proportional to the particle burden and duration of exposure, dividing the disease spectrum into acute (weeks to less than 5 years exposure), accelerated (5 to 10 years exposure), and chronic (greater than 10 years exposure) forms. Progressive massive fibrosis (PMF) represents a macrophage-driven, terminal, and adverse manifestation of silicosis, marked by the presence of extensive, coalescent fibrotic nodules, also known as conglomerate masses, within the lung parenchyma. These large mass-like opacities >1 cm in diametre are the main culprits for the deteriorating nature of the disease despite the efforts with medical management and pose significant challenges in patient outcomes.2
We, herein, report a case of a 38-year male, a stonecutter by profession, with a two-year history of exposure to silica, who developed silicosis, which in a few years led to PMF.
CASE REPORT
A 38-year male, a former stonecutter, a known smoker, normotensive, and non-diabetic, presented in the emergency department with complaints of progressive shortness of breath on exertion, low-grade fever, and dry cough. He had these symptoms for the last five years and was on supportive medication by his local general practitioner. He now presented with worsening of these symptoms. The patient had a two-year-long history of silica dust exposure but left the occupation when he started having symptoms five years back.
On arrival, he was vitally stable with an oxygen saturation of 94% on room air. Auscultation of the chest revealed bilateral wheezes mainly at the upper lung borders. Routine laboratory investigations revealed mild neutrophilic pleocytosis. Blood glucose, renal function tests, liver function tests, serum electrolytes, and coagulation profiles were all within the normal limits. Arterial blood gas analysis showed uncompensated respiratory alkalosis. Sputum for acid-fast bacilli and gene expert was negative. Chest X-ray was indicative of bilateral confluent fibrotic opacities mainly in the upper lung zones, focally extending to the mid zones (Figure 1).
Findings of the high-resolution computed tomography (HRCT) of the chest were typical for PMF in the background of silicosis. It showed large mass-like areas of lung opacification in bilateral upper lobes in peri-hilar distribution with internal air bronchograms and multiple calcifications. Widespread nodular opacities were noted in the vicinity of these areas indicating prior silicosis. Volume loss was present in bilateral upper lobes. Calcification of hilar and mediastinal lymph nodes was also present. In light of the above-mentioned spectrum of radiological findings, the patient was labelled as a case of PMF as a consequence of silicosis.
As there was no specific treatment, the patient was given symptomatic care with antibiotics, bronchodilators, and low-flow oxygen. The patient was counselled about the progressive nature of the disease and was advised to follow-up at regular intervals.
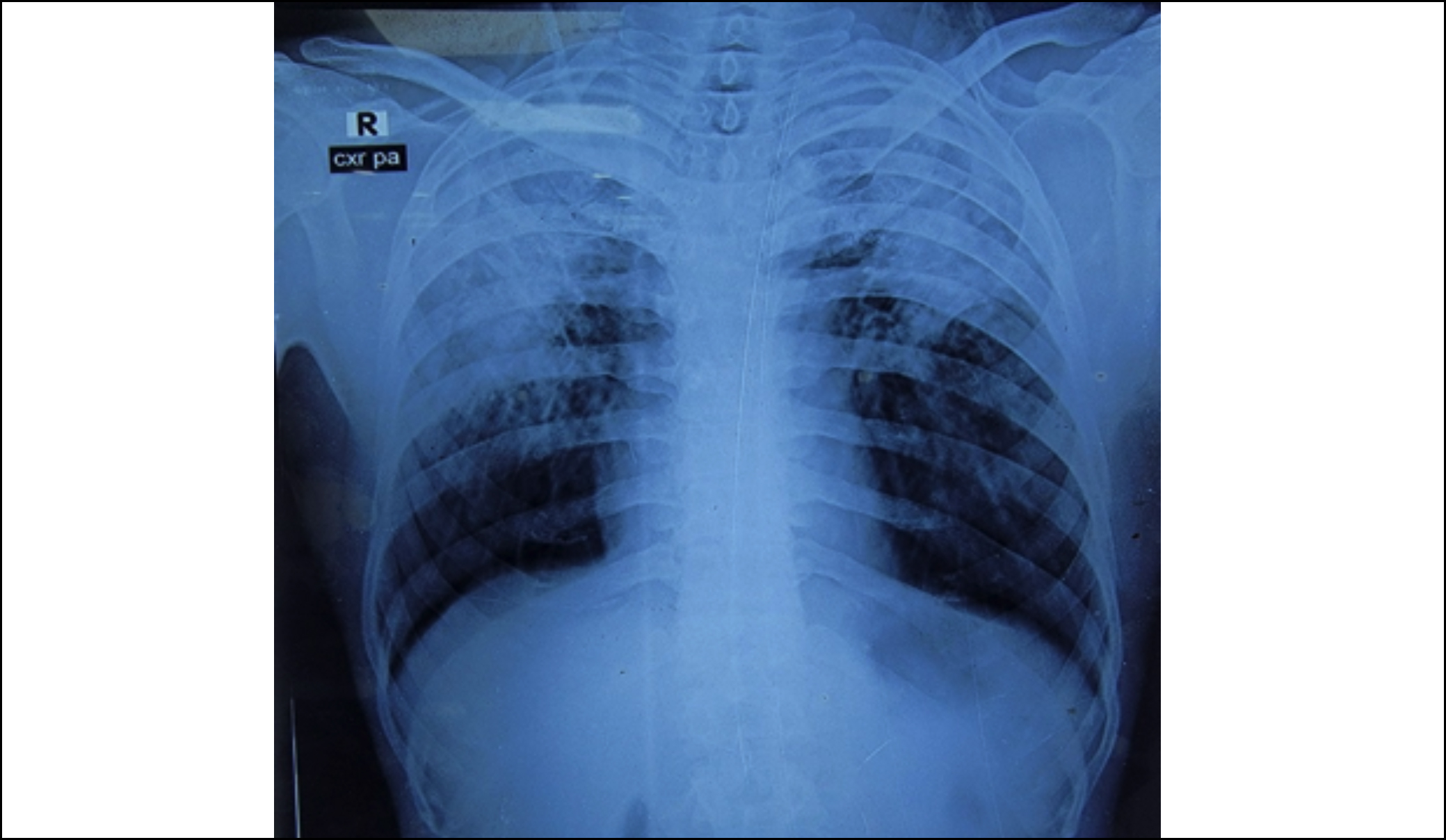 Figure 1: Chest x-ray showing bilateral extensive confluent fibrotic upper lobe opacites.
Figure 1: Chest x-ray showing bilateral extensive confluent fibrotic upper lobe opacites.
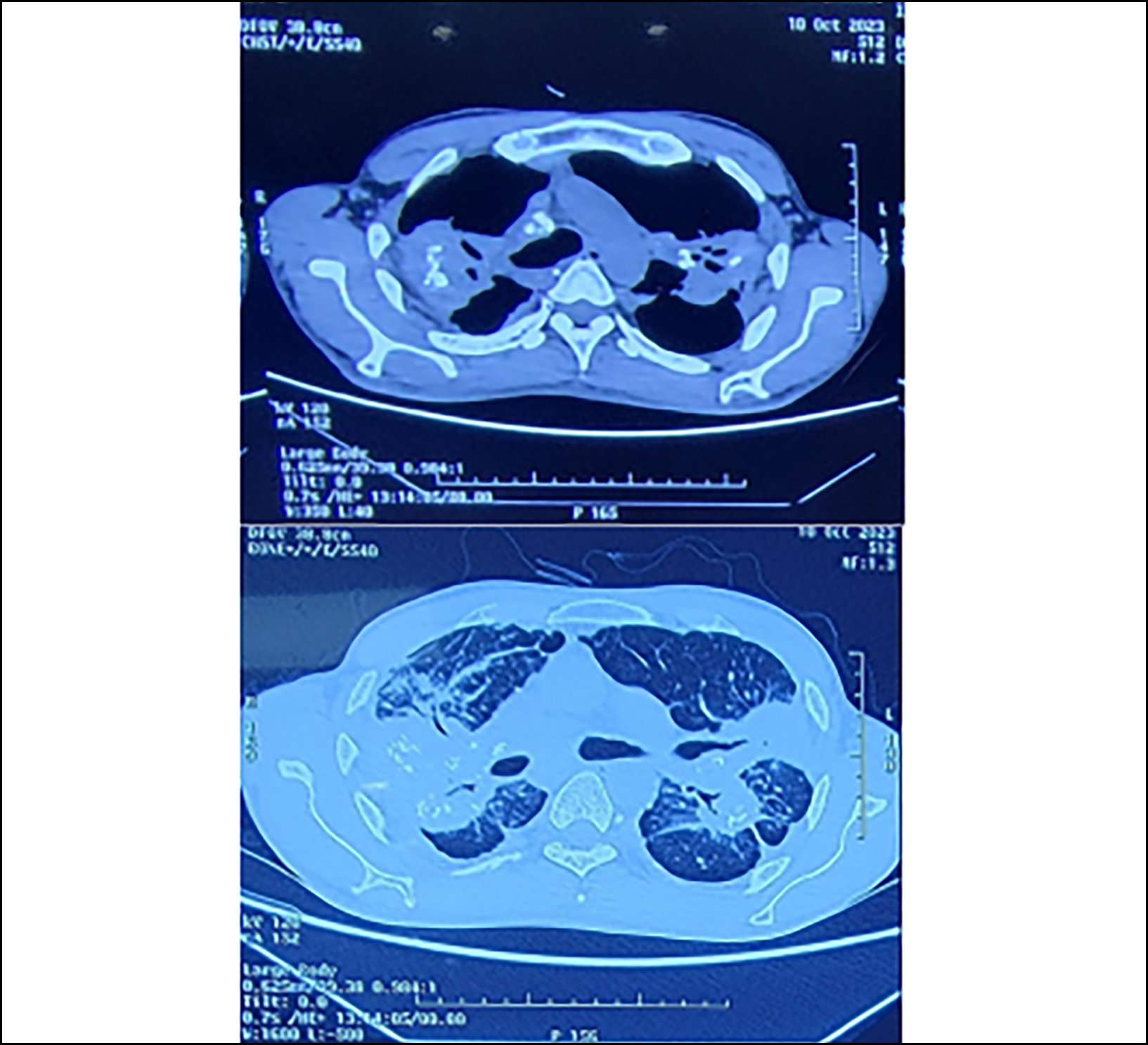 Figure 2: High-resolution computed tomography (HRCT) showing bilateral upper lobe mass-like opacities with adjacent nodules.
Figure 2: High-resolution computed tomography (HRCT) showing bilateral upper lobe mass-like opacities with adjacent nodules.
DISCUSSION
Silicosis is a chronic and progressive occupational lung disease caused by the inhalation of crystalline silica dust. People who work in the mining, quarrying, building, and foundry industries are particularly affected by the condition. The lung parenchyma develops fibrotic nodules over time, which impairs lung function and is the hallmark of silicosis.3 Rarely, silicosis can develop into PMF, a severe and advanced variant, that is marked by enormous coalescent fibrotic masses and poses considerable management difficulties.
Diagnosis and assessment of the severity of PMF mainly depend upon the radiological results. Chest x-ray and HRCT results that are consistent with PMF include substantial bilateral upper lobe opacities and clusters of fibrotic masses, mostly in the upper lung zones. These results denote serious lung damage and advanced disease status, emphasising the significance of aggressive surveillance in high-risk occupational populations.4 Forced vital capacity (FVC), which is measured by pulmonary function tests (PFTs), shows a severe restrictive disease pattern. The patient's quality of life must be managed to the best of one's ability by careful monitoring and the implementation of the necessary measures due to reduced lung function.5
Prevention is the only effective strategy for the control of silicosis and its sequelae.6 To minimise silica dust exposure and associated illness development, it is crucial to implement primary prevention measures such as engineering controls, suitable respiratory protection, and workplace education. Additionally, timely interventions and possibly prevention of the progression to PMF can be aided by routine health surveillance and early identification of silicosis using chest x-rays, particularly among high-risk populations.7
There is currently no known treatment for PMF. The management mostly relies on supportive care. The patient's ability to function properly may be enhanced through pulmonary rehabilitation and oxygen supplementation. As a last resort, lung transplantation may be considered in circumstances where supportive care is unable to improve the patient's quality of life and lengthen survival.
PATIENT’S CONSENT:
Informed consent was obtained from the patient.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
SP, AU, NIB, ZT, MS: Contributed to the design, drafting and critical revision of the manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES